Sleep Apnea
Sleep Apnea Glenn Dale, Greenbelt & Clinton, MD
Sleep apnea is a prevalent sleeping disorder, but it isn’t uncommon for it to go undiagnosed and untreated. At ENT & Sleep Specialists, we have the expertise and technology to offer patients a full spectrum of non-surgical and surgical treatments for Obstructive Sleep Apnea.
What is Sleep Apnea?
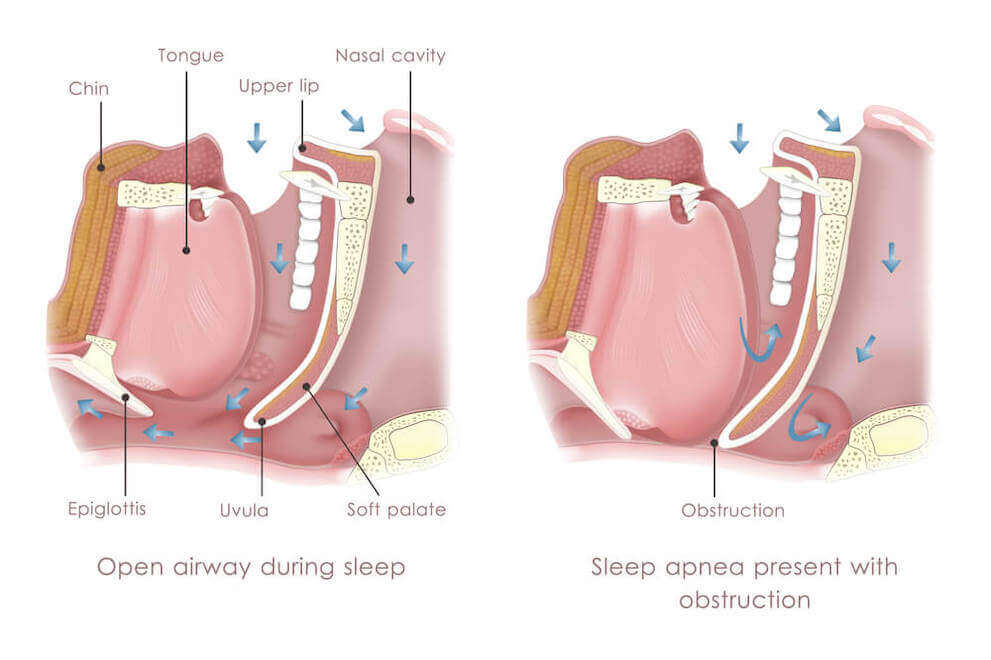
Sleep apnea is a sleeping disorder characterized by abnormal breathing during sleep. There are several different kinds of sleep apnea, but the most common is obstructive sleep apnea (OSA).
It occurs when the airway becomes physically blocked while the patient is sleeping. Luckily, OSA can be treated in a wide variety of ways, both non-invasively and surgically.
Who is at Risk?
There are a few characteristics that can heighten your risk for sleep apnea. The most significant risk factors include:
- Obesity
- Sleeping on your back
- Family history
- Cigarette use
You can also develop sleep apnea due to the shape of your mouth, nose, jaw, tongue, tonsils, or any other part of your body that can obstruct your airway. While you can’t help certain risk factors when it comes to sleep apnea, there are a few things you can control.
Losing weight, quitting smoking, and learning to sleep on your side are standard recommendations for long-term treatment.
Symptoms
It can sometimes be hard to tell whether you have sleep apnea. The primary symptoms of sleep apnea take place while you’re asleep, so they may go unnoticed if you don’t regularly sleep in the same room as another person.
But some common symptoms of sleep apnea, besides snoring and irregular breathing while asleep, are feeling sleepy during the day, poor attention span, irritability, and morning headaches. If you experience these symptoms, you should consider getting tested for sleep apnea, especially if you’re in a high-risk group.
Testing
To be tested for sleep apnea, you need to complete a full sleep study called a nocturnal polysomnography. A nocturnal polysomnography is a sleep study that takes place at a clinic and requires you to sleep hooked up to equipment that monitors your breathing, brain wave patterns, heart rate, oxygen levels, and limb movement while you’re sleeping.
Polysomnography sleep studies can also help diagnose various sleeping disorders, making it ideal if your doctor isn’t sure what’s disrupting your sleep. Sometimes, if your doctor is confident you have sleep apnea, they may administer an at-home sleep test.
This test uses equipment that tests your breathing, heart rate, and oxygen levels. You can administer this test by yourself at home after getting a kit from your doctor.
It’s important to know that at-home sleep tests do not detect all cases of sleep apnea. If the test results indicate that you do have sleep apnea, you can continue with treatment.
However, if the results don’t indicate any abnormalities, your doctor may have you come in for a polysomnography sleep study.
Treatments (Surgical and Non-Surgical)
The most common treatment for sleep apnea is a CPAP or Continuous Positive Airway Pressure machine. This device hooks up to a face mask and delivers air pressure that keeps your airways open while you sleep.
While sleeping with a CPAP machine can take some getting used to, it’s often an effective treatment. There are also oral appliances that can move your jaw forward at night to keep your airway open, as well as other airflow devices.
When these non-invasive treatments aren’t effective, several surgical procedures may help. Some involve implanting a device to keep the airway open or stimulate specific nerves that control tongue movement.
Others involve shrinking or removing tissue from the airway, either the uvula, back of the throat, tonsils, adenoids, or even the tongue. These procedures can be intrusive, but they’re often safe and effective for patients who can’t get relief from sleep apnea from other methods.
Wondering if you or a loved one may have sleep apnea? Schedule an appointment at ENT & Sleep Specialists in Glenn Dale, MD, today!